POTS What Helps?
The contents of this Web page are provided for informational purposes only and should not be used as a substitute for professional medical advice, diagnosis or treatment. Please keep in mind that new treatments are continually emerging and some of the older treatments may rarely be used.
Your physician may prescribe medication to decrease the symptoms of POTS. Doctors admit that treatment can be a challenge and that no single therapy is uniformly successful. Medications that are useful in some patients may have no effect in others. Occasionally medications can worsen symptoms. Medications used to treat POTS include the following:
Anti-arrhythmic drugs, such as disopyramide (norpace), have been used to treat POTS patients. However, studies have shown that some anti-arrhythmic drugs may increase the risk of death, and they are usually used only to treat life-threatening arrhythmias.
Benzodiazepines, such as Clonazepam (klonopin) or alprazolam (xanax), are not used as a first-line of treatment and can worsen tachycardia and hypotension. However, they may be helpful in select patients. Klonapin has been shown to be effective in the treatment of some patients with neurally mediated syncope. These drugs are central nervous system depressants. They are thought to enhance the effect of gaba, an inhibitory neurotransmitter. Benzodiazepines should be used with caution, as they are highly addictive. Some physicians do not advocate their use.
Beta Blockers are especially useful in those with elevated norepinephrine levels, beta-receptor supersensitivity and a hyperadrenergic state. Beta blockers can exacerbate hypotension and are not well tolerated by some dysautonomics. Beta blockers need to be used with caution, as they are known to reduce plasma renin activity. Research shows that hypovolemic orthostatic intolerant patients commonly have inappropriately low levels of plasma renin activity. Reduced plasma renin activity may be an important pathophysiologic component of the syndrome of orthostatic intolerance. Hence, some POTS patients may have low plasma renin activity that is contributing to their disorder. Beta blockers may further lower plasma renin activity in these patients. Therefore, the use of beta blockers in some hypovolemic patients may be counterproductive.
Beta blockers should be used with caution, if at all, in those with mast-cell activation disorders. Beta blockers may trigger mast-cell activation.
Cerefolin is a vitamin supplement that may help patient’s combat fatigue and feel more alert.
Clonidine (Catepres) is a centrally acting alpha-agonist agent. Clonidine inhibits sympathetic outflow. It can stabilize heart rate and blood pressure in patients with post-ganglionic sympathetic involvement. Clonidine will actually display a vasoconstrictive effect in these patients. Clonidine is started at 0.1 mg a day and titrated upward. It is available in a long-acting patch form.
DDAVP (Desmopressin) is used to help patients retain water. DDAVP can raise blood pressure and seems to be especially useful in lessening morning hypotension. It is a man made copy of the anti-diuretic hormone vassopressin. Vassopressin and DDAVP stimulate the kidneys to concentrate urine.
Erythropoietin raises blood pressure and red cell mass. Red blood cell volume has been found to be low in POTS patients. Erythropoietin is also a potent vasoconstrictor and is quite useful in the treatment of orthostatic disorders. There may be an impairment in erythropoietin production and/or function in some individuals with POTS. Erythropoietin reportedly works in 80% of patients. One study showed that erythropoietin administration led to dramatic improvements in some patients with orthostatic hypotension. However, a later study of (only) 8 patients with orthostatic tachycardia reported that erythropoietin did not help the tachycardia. Erythropoietin is not commonly used because it has to be injected and is expensive. Procrit is a common medication that increases erythropoietin, which in turn increases red blood cell mass. Patients treated with erythropoietin may need iron supplementation as their hematocrit rises.
Prior to starting erythropoietin, a complete serum blood count (CBC) as well as a serum iron, total iron binding capacity, and ferritin level should be obtained by one’s physician. Erythropoietin can be employed as long as the hematocrit (HCT) is less than 50, and patients appear to achieve the best hemodynamic effect when the HCT is in the low to mid-40 range. The usual starting dose of erythropoietin is 10,000 units injected subcutaneously once weekly, and it usually takes 4-6 weeks to see the full effects of this medication. Patients should have their HCT checked monthly to make sure it is below 50.
Florinef (Fludrocortisone) increases plasma volume. It helps the body to retain salt and water. It also sensitizes blood vessels so that they can constrict more easily. Some doctors administer salt tablets with florinef. This is because the effectiveness of Florinef depends upon salt intake. Florinef can deplete potassium and magnesium and supplements may be required. Florinef increases intracranial pressure and should not be used in patients with hind brain compression. Numerous symptoms of sympathetic overactivity are enhanced by Florinef and some people develop severe headaches as a result of treatment. Florinef is a mineralocorticoid and, like beta blockers, can reduce levels of plasma renin activity. Reduced levels of plasma renin activity correlate with the hypovolemia observed in some POTS patients. Florinef may be a counterproductive treatment in these patients.
Usually, POTS patients are prescribed 0.1-0.2 mg of fludrocortisone daily. The dose should never exceed 0.4 mg orally each day as adrenal suppression may occur.
Ivabradine, a sinus node blocker, has reportedly helped some POTS patients experience less symptoms. Ivabradine is sometimes used as an alternative to beta-blockers because it results in heart rate reduction without vasodilation, sexual disturbances, ornegative inotropic effects.
Labetalol is sometimes used in POTS patients because it induces both alpha- and beta-blockade. Dosages of 100-400 mg orally twice a day may be employed. Carvedilol works in a similar fashion to labetalol and is also sometimes employed as a treatment for POTS.
Methyldopa is helpful in select POTS patients.
Mestinon (Pyridostigmine Bromide) has traditionally been used to treat myasthenia gravis, but is now sometimes being used to treat POTS patients. Mestinon works by inhibiting the breakdown of acetylcholine. Acetylcholine is the main chemical messenger of the parasympathetic nervous system. Some POTS patients may have immune systems that are mistakenly making antibodies that are plugging up acetylcholine receptors. Mestinon works to unplug these receptors by allowing more acetylcholine to remain at the neuromuscular junction. Mestinon is particulary useful in patients who have the postviral, paraneoplastic or autoimmune forms of POTS. Mestinon is usually started at 30 mg orally twice a day, titrating to 60 mg orally twice daily, if necessary.
Motrin (Ibuprofen) or Indocin (Indomethacin) might be beneficial treatments for patients with postprandial hypotension. Postprandial hypotension refers to low blood pressure occurring after meals. Motrin and indocin block the blood pressure lowering effects of prostaglandins. Studies have suggested that nonsteroidal anti-inflammatory drugs may also lower one’s risk of developing Alzheimer’s disease. However, long term use of nonsteroidal anti-inflammatory drugs can have serious side effects.
Phenobarbital is a central nervous system depressant. It can be useful in the hyperadrenergic form of dysautonomia. However, phenobarbital is a barbiturate and people can become addicted to this drug. Barbiturates can also cause fainting.
Prednisone, plasma exchange or intravenous gamma globulin may be used in patients who are in the acute post-viral phase of the illness. These treatments are most likely to be effective in patients displaying evidence of an acute autonomic neuropathy.
Saline has shown to be very beneficial in decreasing POTS symptoms. It is an inexpensive treatment with few side effects. However, saline must be given through an IV, which is time consuming and may require trips to the doctor’s office. Some of the most severely affected patients report having a peripherally inserted central catheter (PICC line) inserted so that IVs can be administered at home. However, some physicians do not believe the benefits outweigh the possible risks associated with a PICC line.
Selective Serotonin Reuptake Inhibitors (SSRI’s) are sometimes used to treat those with autonomic disorders. SSRI’s are used because serotonin is the principal neurotransmitter that the brain uses to govern autonomic control, in particular to govern blood pressure. Studies have shown that some patients with autonomic disorders may have disturbances in central serotonin production and regulation. SSRI treatment can suppress the sympathetic nervous system. Venlafaxine is particularly effective, possibly due to its actions on norepinephrine as well as serotonin. It has been reported that SSRI’s may be effective in treating the chest pain that is associated with dysautonomia. However, the FDA has issued a public health advisory regarding antidepressants, and they should be used with caution.
Sleep medications are used by some POTS patients. A number of patients have significant sleep disturbances. Some patients report successfully using natural alternatives to sleep medication. Herbal remedies should be used with caution and under a physician’s supervision, as there are known risks with some OTC sleep aids. For example, the FDA has issued warnings regarding Kava Kava and melatonin supplements have been shown to worsen orthostatic intolerance.
Stopping menstruation through the use of birth control pills has reportedly helped some patients feel better. Many women report a worsening of symptoms around menstruation. Stopping menstruation is somewhat controversial, and not all physicians advocate it.
Vasoconstrictors such as ergotamine, midodrine, octreotide, ephedrine, pseudoephedrine, yohimbine, theophylline and ritalin improve venous tone which decreases pooling blood.
Midodrine is particularly useful in patients with peripheral denervation. Midodrine is usually started at 5 mg orally three times a day and can be titrated up to 15-20 mg orally four times a day, if necessary. Midodrine can be used on an as needed basis. Theoretically, continuous use of midodrine could result in constriction of blood volume due to chronic sympathetic activation.
Octreotide is especially useful in preventing vasodilation in the gut, thereby reducing splanchnic pooling. Its actions help to prevent postprandial hypotension (low blood pressure after meals). Octreotide inhibits the release of a variety of gastrointestinal peptides and also may reduce postural and exercise induced hypotension. Octreotide does not often appear to enhance supine nocturnal hypertension, however one study reports that it is a possible side effect.
Octreotide is administered by subcutaneous injection starting at 50 µg 2-3 times a day, and dosages may be titrated up to 100-200 µg three times a day. A long-acting injectable form has also been developed.
Ephedrine is not often used due to its short half-life and undesirable B-adrenergic actions. Ephedrine can cause tachycardia.
Theophyllineis primarily used in asthma patients. One of its effects is to increase vasoconstriction, therefore theophylline is sometimes used to treat dysautonomia.
Ritalin increases peripheral vascular resistance via alpha receptor stimulation. Ritalin is prescribed by some physicians, but can be addictive.
Wellbutrin (Bupropion) is a central nervous system stimulant. It is a dopamine agonist and also a weak blocker of the neuronal uptake of serotonin and norepinephrine. Wellbutrin is not habit forming and works immediately. Wellbutrin can sometimes be used to combat the fatigue that plagues POTS patients.
There are also many non-pharmaceutical methods to decrease the symptoms of POTS. These include the following:
Butcher’s broom may lessen orthostatic hypotension in some patients. Studies show that butcher’s broom does not cause supine hypertension and that it can alleviate the worsening of symptoms in hot environments. Butcher’s broom is a vasoconstrictor that reduces capillary permeability. Butcher’s broom has been used as a diuretic, so patient’s need to be especially cautious about taking it. Butcher’s broom should only be taken under a doctor’s supervision.
Changing eating habits and diet can help relieve hypotension. Patients should eat frequent small meals instead of three large meals a day. This will help reduce the amount of blood needed for digestion. Hence, more blood will be available for the brain and heart. Refined carbohydrates, such as white flour and sugar, can exacerbate hypotension. There are patients that report a worsening of symptoms when eating certain foods, such as dairy products. It is important for each patient to identify and avoid their food triggers.
Cooling devices can help POTS patients. Cool Sport* sells personal body cooling vests that may help patients tolerate hot environments.
Countermaneuvers can help to decrease symptoms by lessening the amount of blood that pools in one’s legs. Useful countermaneuvers include: standing with your legs crossed, sitting in a low chair, sitting in the knee to chest position, leaning forward with your hands on your knees when sitting and tightening the buttocks, thigh and leg muscles when standing (particularly when standing for any length of time). Research shows that tensing the leg muscles while standing enhances brain blood flow and reduces sympathetic activity. Squatting can also be a useful counter-maneuver, although some patients report an increase in symptoms after squatting.
Compression devices, such as abdominal binders and compression stockings, help to reduce the amount of pooling blood. Compression stockings should be at least 30-40 mm Hg and will work best if they are waist high. Compression stockings should be fitted to achieve the greatest benefit. BrightLife Direct* carries affordable compression hosiery.
Correcting anemia has been shown to improve orthostatic tolerance.
Elevating the head of the bed 4-12 inches has helped some POTS patients become less symptomatic. It has been reported that elevating the head of the bed generates mechanisms that expand plasma volume.
Exercise can be helpful to those with dysautonomia. It is important that one does not let their body become deconditioned, as this will exacerbate symptoms. Tightening and building the leg muscles will help them to squeeze pooling blood back to the upper part of the body. Swimming in water has been reported to help many dysautonomics, however no one who faints should go into water alone. Yaz Exercises and recumbent stationary bikes may be beneficial to some patients with POTS. Aerobic exercise performed for 20 minutes a day, three times a week, is sometimes recommended for patients who can tolerate it.
Getting plenty of rest is very important for those with POTS. It has been reported that some POTS patients have significant sleep disturbances. These patients may require more sleep than the average person.
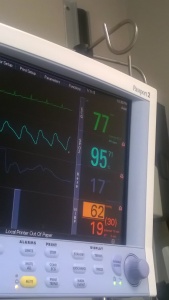
Heart rate watches can help patients identify situations that trigger heart rate increases. These watches are available at sports stores or can be purchased on the Internet.
Ice has reportedly helped some POTS patients. Rubbing ice on the body, especially on the bottom of the feet or neck, may help some POTS patients ward off an episode.
Increasing fluids helps many people with POTS to feel better. Many POTS patients report Gatorade or electrolyte solutions to be particularly helpful. Drinking water has been shown to moderately reduce orthostatic tachycardia in patients with idiopathic orthostatic intolerance. Drinking large amounts of water helps to raise blood pressure. Consuming large amounts of water increases blood volume, which is especially useful in the hypovolemic and those with pooling blood. Some patients report that drinking water before getting out of bed in the morning helps decrease symptoms. Physicians suggest patients drink eight eight-ounce glasses of water daily. Patients should not drink excessive amounts of water because doing so can cause essential electrolytes to become diluted in the bloodstream, which may affect heart rhythm.
Increasing salt is a treatment used for many people with POTS, however salt is not recommended for all patients.
While normal subjects reduce urinary sodium excretion on assumption of upright posture, patients with orthostatic intolerance do so ineffectively. Impaired renal sodium conservation can contribute to hypovolemia. One study found POTS patients to have inappropriately low levels of renin and aldosterone, two hormones that promote sodium retention and increase plasma volume. Renin and aldosterone are both regulated by the kidney.
Increasing salt is an effective way to raise blood pressure in many patients with orthostatic hypotension. Salt helps to expand blood volume. A number of patients find salt tablets and/or electrolyte solutions to be helpful. Some physicians suggest patients who benefit from salt take in 10-15 grams daily. Other physicians suggest between 3-5 grams of salt per day. Salt is 39% sodium, therefore 15 grams of salt equals 5,850 mg of sodium.
Licorice root has been used as a remedy for various disorders throughout history. It can sometimes be used as an alternative to Florinef. Licorice root does have some side effects, and patients should get a physician’s approval before taking it.
Magnesium may be helpful to a number of POTS patients. Magnesium is sometimes prescribed to POTS patients with Ehlers-Danlos syndrome. Some patients report a decrease in arrhythmias after taking this mineral daily for a few weeks. Magnesium deficiency can cause many of the symptoms associated with POTS. Excessive norepinephrine levels can deplete magnesium levels. Magnesium should be used cautiously as it can lower blood pressure.
Scheduling activities in the afternoon as opposed to the morning is a wise decision for those with POTS. Most patients report symptoms being greater in the morning hours.
Sitting down in the shower instead of standing is helpful to many patients. It is important to avoid hot water as this will dilate blood vessels and exacerbate symptoms. Rinsing the legs (or whole body) in cold water before exiting the shower will constrict the blood vessels and should help one to feel less faint.
A sock filled with warmed rice may provide some relief from the headaches that can accompany dysautonomia. Rice socks can be made by filling a tube sock with uncooked white rice, tying the sock closed at the end. Heat the rice filled sock in the microwave for a couple of minutes until warm. Be careful not to overheat, and be cautious of hot spots. The rice will hold heat and provide long-lasting relief of headaches.
Standing up slowly will give a patient’s body more time to adjust to upright posture. Patients getting up from a lying position may find it beneficial to sit up for a few minutes before standing.
Treating allergies might help one to feel better. It has been reported that people with POTS lose their ability to vasoconstrict. This means that many POTS patients have problems with their blood vessels being excessively dilated. Histamine is known to dilate blood vessels, which can further lower blood pressure in POTS patients.
Allergies may also stimulate the sympathetic nervous system. Many POTS patients have overactive sympathetic nervous systems and benefit from avoiding potential sympathetic stimulants.
POTS What To Avoid
Ablation of the sinus node may be detrimental to POTS patients. A Mayo Clinic study reported short-term success in five of seven ablated patients with inappropriate sinus tachycardia and postural orthostatic tachycardia features. However, long-term outcomes were disappointing in these patients. None of the patients experienced complete eradication of symptoms. A follow-up evaluation showed no vast improvement in symptoms, despite better heart rate control. A later publication states “in our laboratory, sinus node modification, total sinus node ablation, or atrioventricular nodal ablation is not recommended for patients with inappropriate sinus tachycardia who have autonomic evidence of postural orthostatic tachycardia”.
Ablations have reportedly been detrimental to some POTS patients who were misdiagnosed as having inappropriate sinus tachycardia. After the apparently successful elimination of their “sinus tachycardia”, they were left with profound orthostatic hypotension.
Alcohol enhances peripheral venous pooling, which will exacerbate hypotension. Alcohol can also lead to a dehydrated state.
Anesthesia can be especially challenging for patients with autonomic dysfunction. When anesthesia is absolutely necessary, an arterial line should be inserted to monitor beat to beat variations in blood pressure. Heart rate should also be constantly monitored, as anesthesia can disturb cardiovascular function. Extra IV fluids are also needed.
Postural orthostatic tachycardia syndrome: anesthetic implications in the obstetric patient: http://www.ncbi.nlm.nih.gov/pubmed/17179264?dopt=AbstractPlus Anaesthetic management of a parturient with the postural orthostatic tachycardia syndrome: a case report: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=16698864&query _hl=1&itool=pubmed_docsum Preoperative considerations in a patient with orthostatic intolerance syndrome: http://journals.lww.com/anesthesiology/pages/articleviewer.aspx?year=2000&issue=08000&article=00041&type=fullte xt Autonomic dysfunction – anaesthetic management http://www.anaesthetist.com/anaes/patient/ans.htm
Bending up and down, as done when picking items up off of the floor, may increase symptoms. It is best to bend at the knee and squat down rather than to bend over forward at the waist.
Blowing up balloons is similar to the valsalva maneuver and can exacerbate symptoms in some patients.
Certain Foods, such as dairy products, may increase symptoms in some patients. White sugar and other refined carbohydrates can exacerbate hypotension by causing increased dilation in the gut. It is important to identify and avoid food triggers. Studies show that gluten sensitivity may play a role in neurological disorders.
Climbing stairs will make some patients feel worse.
Dehydration is one of the worst states a POTS patient can be in. It is very important to always stay well hydrated.
Doctors who don’t know much about POTS will surely leave patients feeling frustrated. Patients of inexperienced doctors may not receive expert care and may not return to optimum health. Finding an experienced physician is not only desirable, it is a necessity.
Eating large meals can worsen hypotension in some individuals with dysautonomia. This is because large meals can cause blood to pool excessively in the abdomen.
Energy Drinks, such as Red Bull, should be avoided in those with POTS. Postural tachycardia syndrome associated with a vasovagal reaction was recorded in a young volleyball player after an excess intake of Red Bull as a refreshing energy drink.
Epinephrine is used by doctors and dentists for a variety of reasons. It is commonly used in numbing shots. It is wise to avoid epinephrine as it stimulates the heart.
Exercise will make many people with dysautonomia feel worse. Strenuous, exhausting exercise should be avoided. Some patients will experience an exacerbation of symptoms after exercise that may last for a day or more, especially if they suffer from mitochondrial disease. These patients should check with a physician before starting any exercise program.
Exercise may be helpful in abating blood from pooling in the limbs. Exercise to build and strengthen the leg muscles can be especially beneficial. Exercise can help POTS patients to avoid becoming deconditioned. A deconditioned state further exacerbates symptoms of orthostatic intolerance.
Fatigue enhances peripheral venous pooling. Those with POTS will do well to live life at their own pace. It is important that patients don’t overdo it, as this will make them feel even worse. POTS will require some lifestyle modification.
Giving blood can be harmful to people with POTS. Blood pooling in the legs already diminishes the amount of blood flowing to the heart and brain. Further, some patients are hypovolemic (have low blood volume) and need every drop of blood that they have. Blood should not be donated and should only be drawn when necessary for medical reasons.
Heat dilates blood vessels and will make POTS symptoms worse. Patients should avoid spending a lot of time outdoors on hot days. POTS patients should not take hot showers/baths or subject their bodies to saunas, hot tubs or greenhouses. Heat enhances peripheral venous pooling.
Holding the arms up in the air can cause problems for some individuals. Holding the arms up requires the heart to work harder to counteract the effects of gravity. This is especially difficult for the heart if there is already excessive venous pooling in the lower limbs. The heart may not be able to effectively pump blood up into raised arms and tachycardia will result from its effort.
Lifting objects can aggravate the symptoms of POTS. This may be due to the increased work load on the heart, especially if blood is pooling in the legs. Pooling blood in the lower body makes less blood available for the muscles in the upper body. Also, straining, bending over, coughing and sneezing all raise cerebral spinal fluid pressure. It has been theorized that some POTS patients may experience symptoms while lifting due to changes in cerebral spinal fluid pressure.
Many medications will affect autonomic testing results. Some medications that have been reported to significantly affect autonomic testing results include: chlorpromazine, thioridazine, tricyclic antidepressants, bupropion, mirtazepine, vanlafaxine, clonidine, alpha blockers, beta blockers, calcium channel blockers, opiates and topical capsaicin. Some physicians believe patients should discontinue measures at alleviating symptoms before autonomic testing. By doing so, symptoms are more likely to present during testing. This may help a physician to discern the true nature of a patient’s disorder.
Numerous over-the-counter products, such as melatonin, can negatively effect the POTS patient. Many products stimulate the heart or lower blood pressure or have diuretic effects, etc. Some products can help one person while hindering another. For example, caffeine can have the positive effect of raising blood pressure in some individuals. However, caffeine also increases the length of time that catecholamines remain active and this can be detrimental to those with a hyperadrenergic state. POTS patients should check with their doctor before taking over-the-counter products.
Over-stimulating environments can make POTS symptoms worse. A number of POTS patients report being overly sensitive to bright lights, loud noises and busy environments.
Singing has been reported to temporarily worsen symptoms in some individuals.
Some pharmacologic agents may cause or worsen orthostatic intolerance. Please check with your physician before taking prescription or over-the-counter medications.
Some of the medications that physicians have identified as causing or worsening orthostatic intolerance include:
Angiotensin Converting Enzyme Inhibitors
Alpha Receptor Blockers
Calcium Channel Blockers
Beta Blockers
Phenothiazines
Tricyclic Antidepressants
Bromocriptine
Ethanol
Opiates
Diuretics
Hydralazine
Ganglionic Blocking Agents
Nitrates
Sildenafil Citrate
MAO Inhibitors
Olanzapine
Stress will often aggravate the symptoms of POTS. The body is continuously adapting to stress, whether it is physical, mental or chemical. POTS patients sometimes lack the ability to correctly process stress due to malfunctioning or excessive functioning of the autonomic nervous system (ANS). Patients may also already have high levels of norepinephrine, which is a stress hormone. POTS patients need to avoid stress (when possible) and live life at their own pace.
Specific stresses such as surgery, childbirth and trauma (such as a car accident) have preceded or worsened the development of POTS in some individuals. This is thought to occur due to a number of factors. Surgery, childbirth and trauma can result in excessive blood loss in POTS patients who may already be hypovolemic. It is important for POTS patients to be given extra fluids during these times. Some people theorize that surgery may require a positioning of the neck that can aggravate hind brain compression. While the relationship between hind brain compression and POTS is controversial, it may be wise to avoid these positions (if possible) with POTS patients. Trauma to the neck may also aggravate hind brain compression. Trauma can result in damage to the ANS and also to areas that will secondarily effect the ANS. Likewise, some believe the straining of bearing down during childbirth can aggravate hind brain compression and effect the ANS. POTS occurring as a result of the nutcracker phenomenon is also more prevalent after childbirth. Hormonal shifts have been theorized to contribute to the development or worsening of POTS symptoms after childbirth as well.
Travel by airplane is challenging for dysautonomics and may increase symptoms. Airplane cabins are pressurized to about 6,500 feet, which is high enough to cause some dysautonomia patients to hyperventilate. Hyperventilating makes a patient more likely to get symptoms of sympathetic activation.
Those with POTS do need to know that the air in an airplane is some of the driest in the world. Flying can have dehydrating effects in normal individuals. How much more so flying might dehydrate someone with low blood volume. Everyone should be well hydrated before boarding a plane. Also, normal people sometimes have trouble with blood pooling in their legs during flights. Rarely, this can lead to the development of blood clots. Patients prone to pooling blood may want to wear compression stockings when flying. Patients may also want to request a bulkhead seat, as this will give them more room to elevate their legs.